
With $262 billion of claims being denied in 2016, data transparency is critical to help identify the reasons for these denials and to prevent similar denials from happening in the future.1
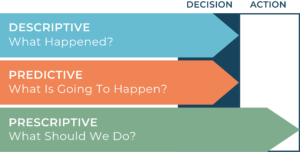
There are three main levels of analysis, each one going deeper into the data than the next: descriptive, predictive, and prescriptive. With each level of analysis comes more visibility into your data and a greater understanding of your denial trends.
The goal of healthcare providers should be to have prescriptive analytics in place so that denials can be limited, leading to a more efficient revenue cycle. However, you cannot approach prescriptive analysis without first achieving the other two levels. We’ll expand on all three levels of analysis, what they entail, and how they can help prevent denials. We’ll also demonstrate each level’s effects on the denial scenario that Prior Authorization was not captured for services.
Descriptive analysis gives an organization the baseline understanding of the data they collect. This is the first step in turning data into actionable insights — allowing you to quantify events and share the insights in an easy to understand way.
This level of analysis helps you understand what your top reasons for denial are, what are the trending of those over time, which areas in an organization that those denials tend to pop up most frequently, and much more. So for the Prior Authorization denial scenario, a descriptive perspective would allow you to report on volume, frequency, and the highest offenders contributing to this type of denial.
Here we have an example of a dashboard that maps out the denials in the past year. You’re able to see the frequency they occurred throughout the year, as well as the top reasons and service lines responsible for denials.
Schedule a demo to see how descriptive analytics can help your organization.
Identifying this basic information is extremely helpful in fully understanding where your organization currently stands in terms of denials. With this data in hand, organizations are able to start breaking it down granularly, leading to the next level of analysis.
Predictive analysis builds from the descriptive analysis. This data is used to predict what may happen in the future, allowing your organization to be more prepared to respond to denials.
This analysis uses statistical models and algorithms to identify patterns in your historical data and to capture relationships between various datasets. You can use these statistics to then forecast what might happen in the future and prioritize based on the findings.
For example, you can categorize denials based on your historical ability to get paid on it. The denials are divided into three categories: high value, mid-range value, and low value. The value that each denial is assigned determines the priority in which it is worked — with high-value denials being worked first, then moving down the line.2
In terms of our failure to obtain Prior Authorization denial scenario, we can use historical data on the frequency of denials by department and payor and likelihood to get paid to identify where to focus efforts from a referral and authorization perspective. Registration and Access workflows are then able to be reviewed to improve documentation and capture of required information.
The final level of analysis is prescriptive analysis. This analysis goes beyond just simply predicting the denial to proactively recommending a way to prevent the denial in the first place.
A majority of healthcare providers are not utilizing prescriptive analysis currently because of the large investment in time and money required to put the systems and processes in place.3 Once an organization is able to use this level of analysis, machine learning may be able to automate the process in the near future, deploying solutions to prevent predicted spikes in denials.
Take our free questionnaire to see how your revenue cycle performance stacks up against other healthcare organizations we work with.
For our Prior Authorization denial scenario, we know where we have a problem because of descriptive analysis and how the data is captured correctly to prevent it due to predictive analysis, so prescriptive analysis tells us exactly where we need to fix the issue and sets in motion actions to fix it promptly instead of retroactively.
Prescriptive analysis is by far the most powerful of the three levels, so naturally, it is the most difficult to achieve. However, once it is achieved, the insights gained are invaluable and can have a massive impact on your organization.
So what does all of this mean in terms of denials? The deeper the level of analysis that your company can achieve, the better chance there is that you can predict and prevent denials from occurring in the future.
Want to learn more about the different levels of analysis and how you can start implementing them in your organization? Contact us and we’ll connect you with one of our revenue cycle experts.
Sources