Situation
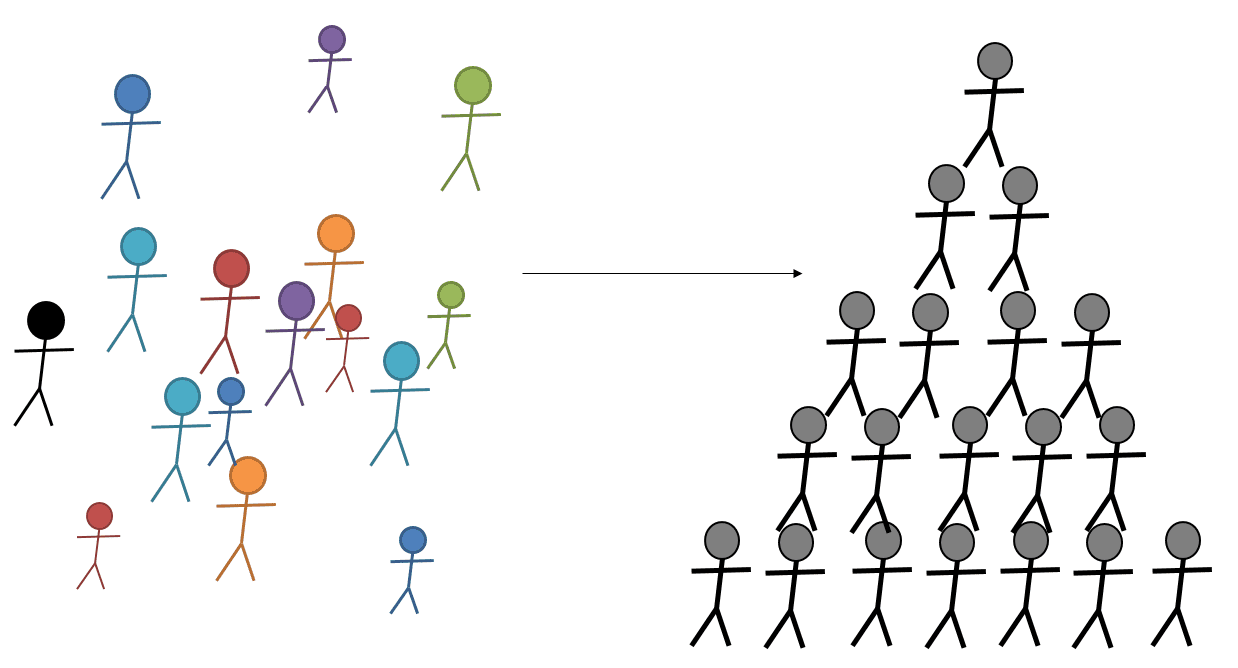
When faced with the challenges arising in the era of value-based care models, many healthcare organizations are reorganizing into Clinical Integration Networks (CINs). A CIN is a legal and organizational designation, grouping primary care and specialty providers with hospital organizations and post-acute facilities. The goal of this organizational alignment is better coordination of care across all patient care settings and reduction of operating costs of care delivery. Prominence worked with a large hospital delivery network as they started on this journey, specifically, to advise and manage the combination of physician, hospital and FQHC billing offices.
Task
In order to successfully facilitate the combination of billing for a new network of providers and facilities, there were a number of foundational tasks we had to tackle including:

Action
During this 18-month engagement:
Result
As a result of the many new structures and EMR build, the customer went live with non-hospital based clinics in August and hospital based clinics in October. The groups are all successfully monitoring KPIs and communicating KPI progress out to the rest of the organization, holding physicians accountable for revenue impacting metrics and setting goals and plans for where they would like to improve and hire. They are basing these decisions on data and metrics they previously couldn’t access.